ShoreOrtho Sports Performance & Injury Prevention Tips A Monthly Blog Series
A Monthly Blog Series
presented by:
Damon A. Greene, MD
Board Certified Orthopaedic Surgeon
Shore Orthopaedic University Associates
October 2020
LABRAL TEARS
ANATOMY
The hip acts as foundation and pivot point for the entire body joining the upper and lower halves. It is just as important for walking as it is for core strength and supporting the upper body.
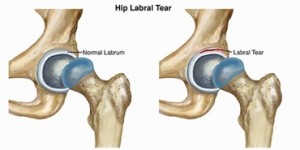
The hip is a ball and socket joint. The head of the ball (femoral head) fits into the socket (the acetabulum). If you imagine a cup the labrum is a thick ring of cartilaginous tissue that surrounds the top of the cup. The labrum has many functions from shock absorber but is two main functions are to confer increased stability to the cup and provide semi airtight seal that helps to keep the synovial fluid in the joint which provides lubrication between the femoral head and acetabulum. The labrum has also been shown to have a collection of nerves and sensory organs which can signal pain if the labrum is damaged. The blood supply to the labrum is very limited which unfortunately limits its ability to heal.
SYMPTOMS
Labral tears are difficult to diagnose, partially because of the many muscles and other structures that are near the hip joint. They are often misdiagnosed as common groin strains and it is not uncommon for the diagnosis to be missed for many months after the labrum is torn
Labral tears are common in athletes and occur when the collagen rips. There are many symptoms of a labral tear. The main symptoms are hip and groin pain. However other symptoms include:
- Pain
- “Catching” feeling in the hip
- Decreased strength
- Decreased range of motion
- Locking of the hip
- Stiffness
 DIAGNOSIS
DIAGNOSIS
Since the diagnosis is difficult a clinical exam by a sports medicine physician or an orthopedic surgeon is the first step. Once the exam is complete the physician may order the following imaging tests:
- X-Rays: X-rays show if there are any problems with the bones such as femeroacetabuluar impingement or osteoarthritis.
- MRI Arthrogram: This test better evaluates the soft tissues around the hip including the labrum.
NONSURGICAL TREATMENT
Hip labral tears can sometimes be treated with nonsurgical treatments. Below are some of the most common.
- Rest. Limited activity is advised to control discomfort, including the activities that bring on hip pain.
- NSAIDs. Taking non-steroidal anti-inflammatory drugs, such as aspirin or ibuprofen, for a limited period may reduce inflammation and pain in the hip area.
- Injections. A doctor may recommend local anesthetic fluid injections directly into the hip joint, called an intra-articular injection. A corticosteroid may be added to the injection depending upon the level of hip pain and any other existing hip problems.
- Physical Therapy. The plan may focus on strengthening the buttocks, thigh, and back, while also improving hip stability. Individuals should consult their doctor before beginning any physical therapy regimen
SURGICAL TREATMENT
If nonsurgical treatments are not recommended, or if they have been tried and do not relieve the hip pain, surgery may be suggested. The type of procedure that will be performed is dependent upon the severity of the tear.
Most surgical options for labral repair are minimally invasive, using a tool called an arthroscope. The arthroscope is about the size of a pencil and equipped with a tiny television camera, allowing the surgeon to view and repair the damaged labrum without having to make a large incision.
- Arthroscopic labral debridement. This technique involves trimming or smoothing the area of the labrum that is torn. This procedure may be recommended if the surgeon believes that a frayed labrum is causing symptoms or could cause future symptoms.
- Arthroscopic hip labral repair. This may be recommended when the labrum has separated from the bone. During a labral repair, the doctor will reattach the torn labrum to the hip’s socket (acetabulum) using small anchors.
Arthroscopic hip labral replacement. Labral replacement, sometimes called labral reconstruction, may be recommended when the labrum is too damaged to repair.
Dr. Greene is a Sports Medicine Fellowship-Trained, Board Certified Orthopaedic Surgeon. He specializes in; acute and chronic ligament, tendon, or cartilage injuries to all major joints; primarily shoulders, elbows, knees and hips. He treats fractures surgically when necessary, but performs casting, bracing, and other non-operative treatments such as specialized injection therapies.




